- PREM NARAYAN MISHRA I am Prem Narayan Mishra . I was Treated for fistula. More … Read More
- SANJIV KUMAR I am Sanjiv Kumar . I was Treated for fistula. More … Read More
- MOHAMMAD AZAM I am Mohammad Azam . I was Treated for fistula. More … Read More
- JAI KUMAR YADAV I am Jai Kumar Yadav . I was Treated for fistula. More … Read More
- R. N. SAROJ I am R. N. Saroj . I was Treated for fistula and piles. … Read More
- MAUNI BABA A patient from Isckon Mauni Baba 98 years male,came … Read More
- RADHA MOHAN I am Radha Mohan. I was Treated for Preoperated and … Read More
- UMESH KUMAR I am Umesh Kumar. I was Treated for fistula completely and … Read More
- SEEMA BEGAM I am Seema Begam. I was suffering from Ulcerative Colitis. … Read More
- SHARDA PRASAD YADAV I am Sharda Prasad Yadav. I was suffering from Fistula. … Read More
- BUDHAI LAL I am Budhai Lal. I was suffering from Fistula. More details … Read More
- VANDNA I am Vandna. I was suffering from Fistula. More details are … Read More
- ROLI SRIVASTAVA I am Roli Srivastava . I was suffering from Fistula. More … Read More
- ANUP CHANDRA MISHRA I am Anup Chandra Mishra . I was suffering from Fistula. … Read More
- K. P. MISHRA I am K. P. Mishra . I was suffering from Ulcerative Colitis.… Read More
- AMIYA ARUN I am Amiya Arun. I was suffering from Fistula. More details … Read More
- PRAKASH SINGH I am Prakash Singh. I was suffering from Fistula. More … Read More
- AARON DAVID I am Aaron David. I was suffering from Fistula. More … Read More
- SAVITA YADAV I am Savita Yadav. I was suffering from Fistula. More … Read More
- SHAMIM AARA I am Shamim Aara. I was suffering from Fistula. More … Read More
- VISHWAS RATHI I am Vishwas Rathi. I was suffering from Ulcerative colitis … Read More
- H. C. SRIVASTAVA I am completely cured by Dr. V.B. Mishra. Below is my … Read More
- SAURABH KESARWANI Great Sir.... I really respect you and regard your … Read More
- DR. PARMESHWAR ARORA Congrats dear.....keep believing in your self.....u can … Read More
- MEENA MISHRA I am Meena Mishra, resident of Allahapur Allahabad. I was … Read More
- ANUJ Thanks a lot doctor for the nice treatment, I am feeling … Read More
Treatment of Crohn's disease in india
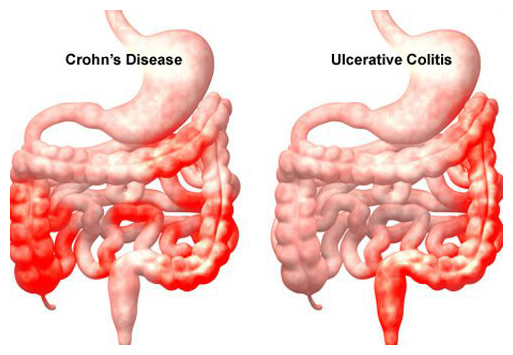
The sites most commonly involved, in order of frequency, are terminal ileum and right side of colon, colon alone, terminal ileum alone, ileum and jejunum. Characteristically, the entire wall of the bowel is oedematous and thickened. There are deep ulcers which often appear as linear fissures; thus the mucosa between them is described as 'cobbleastone'. Deep ulcers may penetrate through the bowel wall to initiate abscesses or fistulae, Fistulae may develop between adjacent loop of bowel or between affected segments of bowel and the bladder, uterus or vagina, and may appear in the perineum.
Characteristically, the changes are the patchy. Even when a relatively short segment od bowel is affected, the inflammatory process is interrupted by island of normal mucosa and the change from the affected part is abrupt. A small lesson separated in this way from a major area of involvement is referred to as a 'skip' lesion. The mesenteric lymph nodes are enlarged and the mesentery thickened.
Histologically, chronic inflammation is seen through all the layers of the bowel wall, which is thickened. There are focal aggregates of epithelioid histiocytes, which may be surrounded by lymphocytes and contain giant cells. Lymphoid aggregates or microgranulomas are also seen, and when these are near to the surface of the mucosa they often ulcerate to form tiny apthous-like ulcers.
Clinical features symptoms of crohn's disease
The major symptoms are abdominal pain, diarrhoea and weight loss.
Ileal crohn's disease causes abdominal pain, principally because of subacute intestinal obstruction, although an inflammatory mass, intra-abdominal abscess or acute obstruction may be responsible. Pain is often associated with diarrhoea which is watery and does not contain blood or mucus. Almost all patients lose weight. This is usually because they avoid food since eating provokes pain. Weight loss may also be due to malabsorption, and some patients present with features of fat, protein or vitamin deficiencies.
Crohn's colitis presents in an identical manner to ulcerative colitis, with bloody diarrhoea, passage of mucus and constitutional symptoms including lethargy, malaise, anorexia and weight loss. Rectal sparing and the presence of perianal disease are features which favour a diagnosis of Crohn's disease rather than ulcerative colitis.
Many patients present with symptoms of both small bowel and colonic disease. A few have isolated perianal disease, vomiting from jejunal strictures or severe oral ulceration.
Physical examination often reveals evidence of weight loss, anaemia with glossitis and angular stomatitis. There is abdominal tenderness, most marked over the inflamed area. An abdominal mass due to matted loops of thickened bowel or an intra-abdominal abscess may occur. Perianal skin tags, fissures or fistulae are found in at least 50% of patients.
Complications of crohn's disease
Severe, life-threatening inflammation of the colon. This occurs in both ulcerative colitis and Crohn's disease. In the most extreme cases the colon dilates (toxic megacolon) and bacterial toxins pass freely across the diseased mucosa into the portal then systemic circulation. This complication occurs most commonly during the first attack of colitis. An abdominal X-ray should be taken daily because when the transverse colon is dilated to more than 6cm there is a high risk of colonic perforation.
Perforation of the small intestine or colon. This can occur without the development of toxic megacolon.
Life-threatening acute haemorrhage. Haemorrhage due to erosion of a major artery is a rare complication of both conditions.
Fistulae and perianal disease. Fistulous connections between loops of affected bowel, or between bowel and bladder or vagina are specific complications of Crohn's disease and do not occur in ulcerative colitis. Enteroenteric fistulae cause diarrhoea and malabsorption due to blind loop syndrome. Enterovesical fistulation causes recurrent urinary infections and pneumaturia. An enterovaginal fistula causes a feculent vaginal discharge. Fistulation from the bowel may also cause perianal or ischiorectal abscesses, fissures and fistulae. These may sometimes be extremely severe and can be the source of great morbidity.
Cancer. Patients with extensive active colitis of more than 8 years' duration are at increased risk of colon cancer. The cumulative risk for ulcerative colitis may be as high as 20% after 30 years but is probably lower for Crohn's colitis. Tumours develop in areas of dysplasia and may be multiple. Small bowel adenocarcinoma is a rare complication of long-standing small bowel Crohn's disease. Patients with long-standing, extensive colitis are therefore entered into surveillance colonoscopy programmes beginning 8-10 years after diagnosis. Multiple random biopsies are taken...
Small bowel Crohn's disease
Crohn's disease can usually be diagnosed with confidence without histological confirmation in the appropriate clinical setting. Indium- or technetium-labelled white cell scanning may help identify inflamed intestinal segments. In atypical cases biopsy or surgical resection is necessary to exclude other diseases. This can often be done endoscopically by ileal intubation at colonoscopy, but sometimes laparotomy or laparoscopy with resection or full-thickness biopsy is necessary.
Crohn's disease
The indications for surgery are similar to those for ulcerative colitis. Operations are often necessary to deal with fistulae, abscesses and perianal disease, and may also be required to relieve small or large bowel obstruction.
In contrast to ulcerative colitis, surgery is not curative and disease recurrence is the rule. Surgical intervention should therefore be as conservative as possible in order to minimise loss of viable intestine and to avoid creation of a short bowel syndrome.
Obstructing or fistulating small bowel disease may require resection of affected tissue. Patients who have localised segments of Crohn's colitis may be managed by segmental resection and/or multiple stricturoplasties in which the stricture is not resected but instead incised in its longitudinal axis and sutured transversely. Others who have extensive colitis require total colectomy but ileal-anal pouch formation should be avoided because of the high risk of disease recurrence within the pouch and subsequent fistulae, abscess formation and pouch failure.
Patients who have perianal Crohn's disease are managed as conservatively as possible. Seton drainage, fistulectomy and use of advancement flaps are appropriate for complex fistulae in combination with medical therapies.
Google Reviews - View All Google Reviews